Max was a four-year-old Border Collie who spun in circles. Not playful zoomies—obsessive, relentless spinning that left worn patches in the carpet. His owner, Rachel, had tried everything: a certified behaviorist, desensitization protocols, anti-anxiety medication. Nothing worked. Max was labeled "untrainable."
Then Rachel's new vet asked an unexpected question: "What does his poop look like?"
It turned out Max had been on multiple courses of antibiotics as a puppy for chronic ear infections. His gut was destroyed. When they finally addressed his microbiome, the spinning stopped within six weeks.
Max wasn't stubborn. Max wasn't broken. Max was inflamed.
This is the story of the Gut-Brain Axis—the hidden highway connecting your dog's intestines to their behavior. If you have tried training, medication, and environmental management without success, this article might hold the missing piece of the puzzle.
In This Guide:
- Part 1: Anatomy of the Axis (The Vagus Nerve & Enteric Nervous System)
- Part 2: How the Gut Creates Anxiety (Dysbiosis, Leaky Gut, Neuroinflammation)
- Part 3: Diagnosing the "Anxious Gut" (The Red Flags)
- Part 4: The Saboteurs (Antibiotics, Stress, Diet)
- Part 5: Psychobiotics (The Mood-Altering Microbes)
- Part 6: The 4R Protocol (Remove, Replace, Reinoculate, Repair)
- FAQ: Gut-Brain Axis Questions
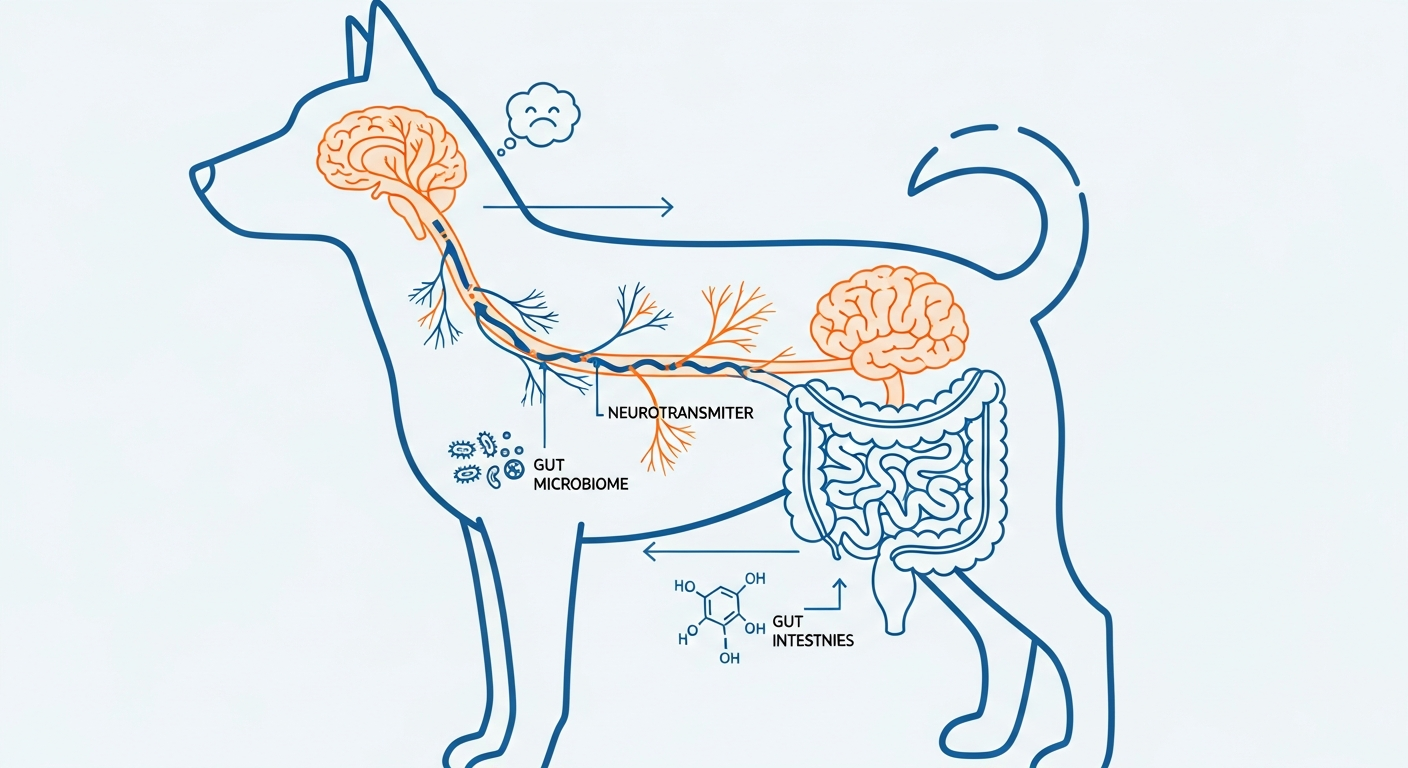
Part 1: Anatomy of the Axis (The Vagus Nerve & Enteric Nervous System)
To understand why your dog's gut can make them anxious, you first need to understand the anatomy of the communication system between the belly and the brain.
The Vagus Nerve: The "Information Superhighway"
The Vagus Nerve is the longest cranial nerve in the body. It runs from the brainstem all the way down through the chest and into the abdomen, touching nearly every major organ along the way—including the entire digestive tract.
Think of it as a two-way fiber optic cable. It carries messages down from the brain ("Slow down digestion, we're stressed!") and messages up from the gut ("Hey brain, we're detecting some bad bacteria down here...").
Here's the critical fact: Approximately 80-90% of the signals traveling along the Vagus Nerve go up—from the gut to the brain. That means your dog's gut is constantly broadcasting information to their brain, shaping their mood, their stress response, and their behavior.
When the gut is healthy, it sends "all clear" signals. When the gut is inflamed or imbalanced, it sends alarm signals. Those alarms manifest as anxiety, reactivity, and obsessive behaviors.
The Enteric Nervous System: The "Second Brain"
Your dog has roughly 500 million neurons lining their gut. This is called the Enteric Nervous System (ENS), and it is so complex that scientists call it the "Second Brain."
The ENS can operate independently of the brain. It controls digestion, motility, and even immune responses. But it also produces neurotransmitters—the same chemicals that the brain uses to regulate mood.
The Serotonin Connection: You've probably heard of Serotonin as the "happiness hormone." What most people don't know is that approximately 90% of the body's Serotonin is produced in the gut, not the brain. The bacteria living in your dog's intestines directly influence how much Serotonin is manufactured and released.
A dog with a damaged microbiome literally cannot produce enough of the neurotransmitter they need to feel calm. No amount of training can fix a neurochemical deficit.
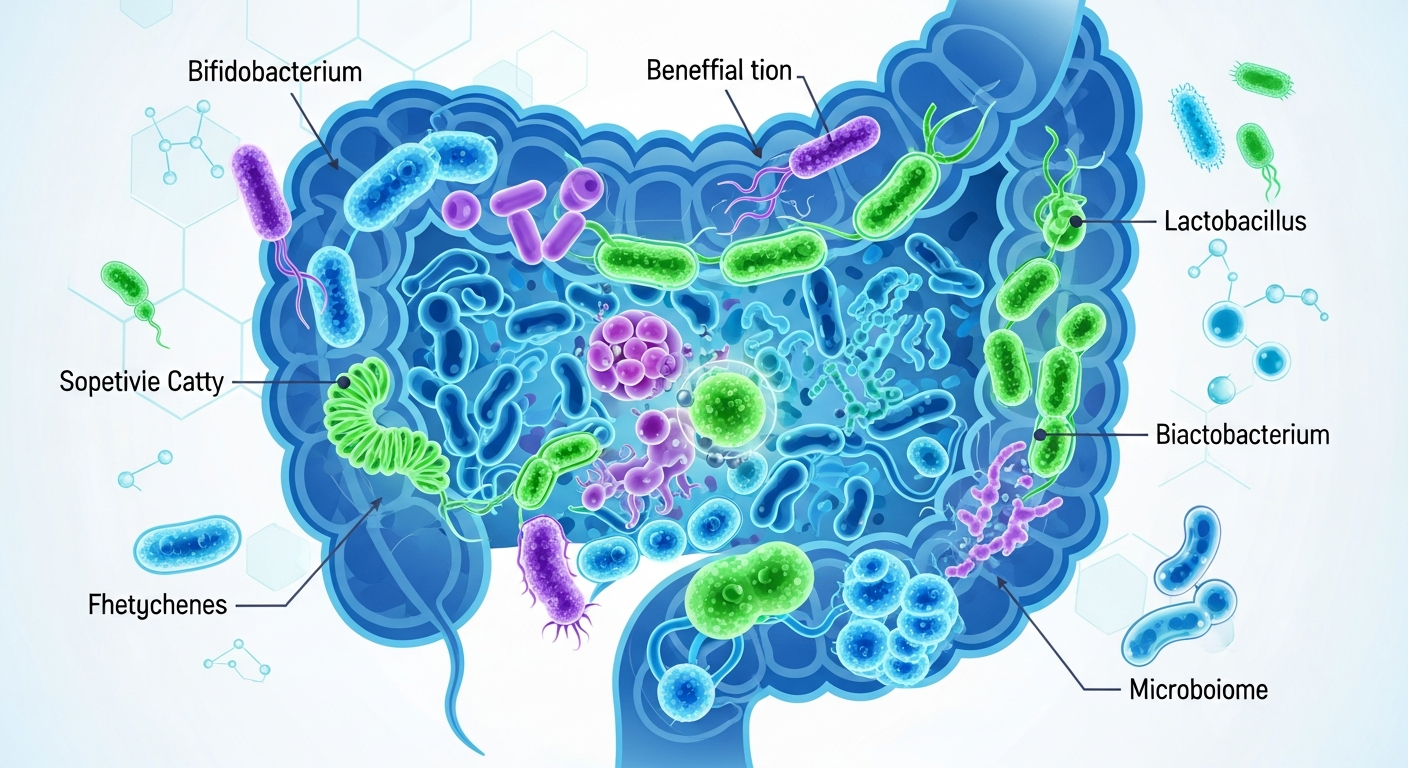
The Microbiome: The "Control Room"
Living inside your dog's gut are trillions of microorganisms—bacteria, fungi, viruses, and protozoa. This community is called the Microbiome. The balance of species in this community determines whether the gut sends calming signals or panic signals up the Vagus Nerve.
A healthy microbiome is diverse. It contains a wide variety of beneficial species that work together to digest food, produce vitamins, regulate inflammation, and manufacture neurotransmitters.
An unhealthy microbiome—called Dysbiosis—is like a city where the police force has been replaced by gangs. Harmful bacteria overgrow, beneficial bacteria die off, and the gut starts sending distress signals to the brain around the clock.
Part 2: How the Gut Creates Anxiety (Dysbiosis, Leaky Gut, Neuroinflammation)

Now that you understand the anatomy, let's trace the exact mechanism by which a damaged gut creates an anxious dog. This is a cascade—one problem leads to the next.
Step 1: Dysbiosis (The Bacterial Imbalance)
Dysbiosis is the medical term for an imbalance in the gut microbiome. It happens when harmful bacteria outcompete beneficial bacteria. The causes are numerous (we'll cover them in Part 4), but the result is the same: the gut's internal ecosystem collapses.
When dysbiosis sets in, several bad things happen simultaneously:
- Reduced Serotonin Production: Beneficial bacteria like Lactobacillus and Bifidobacterium are responsible for stimulating Serotonin production. When they die off, Serotonin levels plummet.
- Increased Cortisol: Harmful bacteria release toxins that trigger the stress response. Cortisol levels rise chronically.
- GABA Disruption: GABA is the brain's "calming" neurotransmitter. Certain gut bacteria produce GABA directly. Without them, the brain becomes hyperexcitable.
Step 2: Leaky Gut (Intestinal Permeability)
The gut lining is supposed to act like a cheesecloth—allowing nutrients through while keeping pathogens and undigested food particles out. But when the gut is inflamed (from dysbiosis, poor diet, or chronic stress), the "tight junctions" between cells start to loosen.
This is called "Leaky Gut" or Intestinal Permeability. Now, molecules that should stay inside the intestines leak into the bloodstream. The immune system sees these foreign invaders and sounds the alarm.
The result? Systemic inflammation. The entire body—including the brain—enters a state of chronic low-grade immune activation.
Step 3: Neuroinflammation (The Brain on Fire)
When inflammatory signals from a leaky gut reach the brain, they trigger neuroinflammation. The brain's immune cells (called microglia) become hyperactive. They release inflammatory cytokines that alter neurotransmitter function and neural plasticity.
Studies in both humans and animals have shown that neuroinflammation is directly linked to:
- Anxiety and fear responses
- Depression and learned helplessness
- Obsessive-compulsive behaviors (like spinning, tail chasing, and excessive licking)
- Aggression and reactivity
This is why Max was spinning. It wasn't a "training problem." It was inflammation in his brain, triggered by inflammation in his gut, caused by antibiotics that destroyed his microbiome years earlier.
The Vicious Cycle
Here's where it gets worse: Anxiety itself damages the gut. When a dog is chronically stressed, their body diverts blood away from the digestive system (Fight or Flight mode). Digestion slows. The gut lining becomes more permeable. Beneficial bacteria die off because the environment becomes hostile.
This creates a vicious feedback loop:
Dysbiosis → Leaky Gut → Neuroinflammation → Anxiety → More Stress → Worsening Dysbiosis → Repeat.
To break the cycle, you have to intervene at the gut level. You cannot train your way out of a biological feedback loop.
Part 3: Diagnosing the "Anxious Gut" (The Red Flags)
How do you know if your dog's anxiety is coming from their gut? There is no single test that gives you a definitive answer, but there are red flags that suggest the gut-brain axis is involved.
Red Flag #1: History of Antibiotics
Has your dog been on multiple courses of antibiotics—especially as a puppy? Antibiotics are nuclear bombs for the microbiome. They kill pathogens, but they also kill beneficial bacteria. The gut can take months or years to recover, and sometimes it never fully bounces back without intervention.
If your anxious dog has a history of ear infections, urinary tract infections, skin infections, or any condition requiring repeated antibiotic use, the gut-brain connection is worth investigating.
Red Flag #2: Chronic Digestive Issues
Does your dog have any of the following?
- Loose stools or chronic diarrhea
- Excessive gas or bloating
- Constipation
- Vomiting bile (especially in the morning)
- Grass eating
- Inconsistent appetite
These symptoms suggest the gut is already compromised. A dog with obvious digestive dysfunction is almost certainly experiencing some degree of dysbiosis.
Red Flag #3: Skin and Allergy Problems
The skin is the largest organ of the body, and it is intimately connected to gut health. If your dog has chronic itching, hot spots, yeast infections (especially in the ears or paws), or environmental allergies, the root cause is often a leaky gut allowing inflammatory compounds into the bloodstream.
There's even a term for this: the "Gut-Skin Axis." Inflammation in the gut manifests as inflammation on the skin. If your dog is both anxious AND itchy, the gut is the prime suspect.
Red Flag #4: Anxiety That Doesn't Respond to Traditional Treatment
This is the hallmark sign. You've tried:
- Counterconditioning and desensitization
- Anti-anxiety medications (Trazodone, Fluoxetine, etc.)
- Environmental management
- Exercise and mental stimulation
...and your dog is still a mess. If the usual toolkit isn't working, it's a strong signal that something deeper is driving the anxiety. The gut is the most overlooked piece of that puzzle.
Red Flag #5: Obsessive-Compulsive Behaviors
Spinning, tail chasing, flank sucking, excessive licking (especially of paws or surfaces), fly snapping at invisible objects—these are all classified as Canine Compulsive Disorders (CCD). Research strongly links these behaviors to neuroinflammation and serotonin dysfunction, both of which are influenced by gut health.
Part 4: The Saboteurs (What Destroys the Microbiome)
Understanding what damages the gut is crucial for prevention and treatment. Here are the primary saboteurs of your dog's microbiome.
Saboteur #1: Antibiotics
We've already mentioned this, but it bears repeating. A single course of antibiotics can reduce microbiome diversity by up to 50%. While the gut does partially recover, some species may be permanently lost.
The Fix: If antibiotics are medically necessary, always follow up with a course of probiotics and prebiotics to help repopulate the gut. Start probiotics during the antibiotic course (spaced 2 hours apart from the medication) and continue for at least 30 days after.
Saboteur #2: Chronic Stress
Stress is not just psychological—it is physiological. When a dog is chronically stressed (from separation anxiety, noise phobias, or living in a chaotic environment), their cortisol levels remain elevated. Cortisol directly alters the gut environment, killing beneficial bacteria and allowing pathogens to flourish.
Studies have shown that dogs in shelters (high-stress environments) have significantly different microbiomes than dogs in stable homes. Stress literally reshapes the gut.
Saboteur #3: Ultra-Processed Diet
Most commercial kibble is heavily processed, high in carbohydrates, and low in fiber diversity. The gut microbiome evolved to thrive on whole foods—meat, bones, organs, and a variety of plant fibers. A monotonous diet of the same kibble every day starves the beneficial bacteria that need diverse fibers to survive.
The research is clear: Dogs fed fresh, whole-food diets have more diverse and healthier microbiomes than dogs fed exclusively on kibble. This doesn't mean you have to go fully raw—but adding fresh food toppers (cooked vegetables, fermented foods, bone broth) can make a significant difference.
Saboteur #4: NSAIDs and Other Medications
Non-steroidal anti-inflammatory drugs (like Rimadyl or Metacam), proton pump inhibitors (antacids), and steroids (like Prednisone) all have documented negative effects on the gut microbiome. If your dog is on long-term medication for arthritis, allergies, or chronic pain, the gut may be taking collateral damage.
Saboteur #5: Early Life Disruption
Puppies acquire their initial microbiome from their mother—through the birth canal and through nursing. Puppies who were born via C-section, separated from their mother too early, or bottle-fed may have a compromised microbiome from the start.
This early-life disruption has lifelong consequences. It's one reason why puppy mill dogs often have chronic digestive issues and anxiety—they never got the microbial "starter kit" they needed.
Part 5: Psychobiotics (The Mood-Altering Microbes)
Psychobiotics is a term coined by researchers to describe specific strains of probiotics that have documented effects on brain function and mental health. Not all probiotics are psychobiotics. You need the right strains.
The Star Players
Bifidobacterium longum BL999
This is one of the most researched strains for anxiety reduction in dogs. A landmark study by Purina found that dogs supplemented with BL999 showed significantly reduced cortisol levels, reduced heart rate during stressful events, and less anxious behaviors (barking, jumping, spinning, pacing) compared to the control group.
The effect size was comparable to some anti-anxiety medications—without the side effects.
Lactobacillus rhamnosus
This strain has been shown to influence GABA receptors in the brain via the Vagus Nerve. Studies in mice showed that L. rhamnosus reduced anxiety-like behaviors and lowered stress-induced corticosterone (the rodent equivalent of cortisol). When researchers cut the Vagus Nerve, the effect disappeared—proving that the gut-brain communication was essential.
Lactobacillus helveticus and Bifidobacterium longum (Combination)
This combination has been studied in humans for anxiety and depression, with significant results. While direct canine studies are limited, the mechanism is the same across mammals, and many veterinary behaviorists now recommend this combination for anxious dogs.
How to Choose a Probiotic
Not all pet probiotics are created equal. Many cheap products contain dead bacteria (CFU counts are useless if the bugs don't survive shipping and stomach acid) or strains that have no research behind them.
What to look for:
- Strain-specific labeling (e.g., "Bifidobacterium longum BL999," not just "Bifidobacterium longum")
- Third-party testing for viability
- Enteric coating or packaging designed to survive stomach acid
- Research backing the specific strains included
Part 6: The 4R Protocol (Remove, Replace, Reinoculate, Repair)
Functional medicine practitioners use a framework called the "4R Protocol" to heal the gut. This structured approach addresses the root causes of dysbiosis and leaky gut systematically. Here's how to apply it to your dog.
Step 1: REMOVE
The first step is to remove anything that is damaging the gut or feeding harmful bacteria.
Remove:
- Inflammatory foods: Identify and eliminate any foods your dog is intolerant to. Common culprits include chicken, beef, wheat, corn, and soy. An elimination diet (feeding a novel protein like venison or rabbit for 8-12 weeks) can help identify triggers.
- Unnecessary medications: Work with your vet to taper off any medications that are not essential. If NSAIDs or steroids are needed, discuss gut-protective strategies.
- Environmental stressors: Reduce chronic stress as much as possible. This might mean management strategies like white noise for sound-sensitive dogs, or desensitization work for separation anxiety.
Step 2: REPLACE
Replace what the gut is missing to function properly.
Replace:
- Digestive enzymes: Many dogs with compromised guts don't produce enough enzymes to properly break down food. Adding a digestive enzyme supplement can improve nutrient absorption and reduce undigested food particles that feed bad bacteria.
- Stomach acid support: Contrary to popular belief, many dogs have LOW stomach acid (hypochlorhydria), not high. This leads to poor protein digestion and allows pathogens to survive into the intestines. Apple cider vinegar (1 tsp per 20 lbs of body weight, diluted in water and added to food) can help.
- Bile salts: For dogs with fat malabsorption or who have had their gallbladder removed.
Step 3: REINOCULATE
This is where probiotics come in. But we're not just throwing random bugs at the problem—we're strategically repopulating with beneficial species.
Reinoculate with:
- High-quality probiotics: Look for the psychobiotic strains mentioned above (BL999, L. rhamnosus). Give for at least 60-90 days to allow colonization.
- Prebiotics: Prebiotics are fibers that feed beneficial bacteria. Sources include: inulin, chicory root, Jerusalem artichoke, green banana flour, and cooked (then cooled) potatoes or rice (which creates "resistant starch").
- Fermented foods: A small amount of raw goat milk kefir, sauerkraut juice (no onions or garlic), or plain unsweetened yogurt can introduce live cultures.
Step 4: REPAIR
Finally, repair the damaged gut lining to seal the "leaky gut."
Repair with:
- L-Glutamine: This amino acid is the primary fuel source for intestinal cells. It helps rebuild the gut lining. Dose: approximately 500mg per 20 lbs of body weight, once daily.
- Bone broth: Homemade bone broth (simmered 24-48 hours) contains collagen, gelatin, and glycine—all essential for gut repair. Give 1-4 oz daily depending on size.
- Slippery Elm: This herb forms a soothing gel that coats and protects the gut lining. It's particularly helpful for dogs with chronic diarrhea or irritable bowel.
- Marshmallow Root: Another mucilaginous herb that protects and heals the intestinal mucosa.
- Omega-3 Fatty Acids: Fish oil reduces inflammation throughout the body, including the gut. Use a high-quality marine-sourced oil (salmon, sardine, or anchovy).
Timeline: What to Expect
Gut healing is not overnight. Here's a realistic timeline:
- Week 1-2: You may see initial changes in stool quality (better formed, less odor). Some dogs experience a brief "detox" period with slightly loose stools as bad bacteria die off.
- Week 3-6: Digestive improvements stabilize. You may notice subtle behavior changes—slightly calmer, sleeping better, less reactive on walks.
- Week 6-12: This is when the magic happens. As neuroinflammation decreases and neurotransmitter production normalizes, significant behavior changes become apparent. The anxious behaviors that didn't respond to training may finally start to shift.
- Month 3-6: Long-term microbiome remodeling. Continue the protocol with a maintenance dose of probiotics and ongoing dietary support.
Important: Do not abandon the protocol after 2-3 weeks if you don't see immediate behavior changes. The gut-brain connection takes time to heal. Commit to at least 90 days before evaluating results.
FAQ: Gut-Brain Axis Questions
Q: Can I just give my dog yogurt instead of probiotics?
A: Yogurt contains beneficial bacteria, but the strains and quantities are typically not sufficient for therapeutic gut repair. It can be a helpful supplement, but for a dog with significant dysbiosis, you need a high-potency, strain-specific probiotic. Think of yogurt as "maintenance" and probiotics as "treatment."
Q: My dog is on anti-anxiety medication. Can I still do this protocol?
A: Absolutely. The 4R Protocol is complementary to pharmaceutical treatment—not a replacement. In fact, healing the gut may allow you to eventually reduce medication doses (under veterinary supervision). Do not stop prescribed medications without consulting your vet.
Q: How do I know if my dog has Leaky Gut?
A: There is no simple at-home test for leaky gut. However, if your dog has chronic digestive issues, skin problems, multiple food sensitivities, and/or anxiety that doesn't respond to treatment, intestinal permeability is highly likely. Some veterinary labs offer Zonulin testing (a marker of leaky gut), but it's not widely available. Treating empirically with the 4R Protocol is often the practical approach.
Q: Should I do a microbiome test?
A: Microbiome testing (like AnimalBiome's Gut Health Test) can be valuable for identifying specific imbalances and tracking progress. It's not strictly necessary to start the protocol, but it can provide useful baseline data and guide targeted interventions.
Q: My vet has never mentioned the gut-brain connection. Is this real science?
A: Yes. The gut-brain axis is well-established in the scientific literature—it's just slow to reach mainstream veterinary practice. If your vet is unfamiliar, you can reference studies from journals like "Gut Microbes," "Frontiers in Behavioral Neuroscience," and research from the American Kennel Club Canine Health Foundation. Many veterinary behaviorists and integrative vets are now incorporating gut health into anxiety treatment plans.
Q: How long do I need to continue the protocol?
A: The intensive phase (full 4R Protocol) typically lasts 3-6 months. After that, transition to a maintenance phase: continue feeding a diverse, whole-food diet, give probiotics 3-4 times per week (instead of daily), and add bone broth a few times per week. The gut is a living ecosystem—it needs ongoing support.
Summary: The Hidden Key
When Rachel first heard that her dog's spinning might be related to his gut, she was skeptical. It sounded like pseudoscience. But after months of failed training protocols and medication trials, she was willing to try anything.
Six weeks into the 4R Protocol, Max stopped spinning.
Not "reduced" spinning. Stopped. The behavior that had defined his life for years—the behavior that multiple professionals had called "intractable"—disappeared once his gut healed and the inflammation in his brain resolved.
This isn't magic. It's biology. The gut and the brain are connected in ways we are only beginning to understand. For some dogs, the key to unlocking calm behavior isn't in their head—it's in their belly.
If training has failed, if medication has failed, if you've tried everything... look to the gut. The answer might be hiding in plain sight.